End-of-Year Sale: Subscribe by December 31 to Get 3 Months Free!
Learn More
Table of Contents

Experience Better Practice Management Today!
Starting at $28.05/month
No Credit Card Required

Experience Better Practice Management Today!
Starting at $30/month
No Credit Card Required
Is your practice hemorrhaging money through billing gaps? You're not alone.
Every denied claim is revenue you’ve already earned but can’t collect.
The good news? Most billing issues are preventable. With the right approach, you can cut denials, speed up reimbursements, and simplify your entire process.
Below, you’ll find practical chiropractic billing tips to fix common mistakes, reduce rejections, and improve cash flow. A few smart changes can turn billing from a hassle into a smooth, predictable process. Let’s get started.
Every billing mistake costs money. Whether it’s claims not submitted, coding errors, or delayed follow-ups, these issues create revenue leaks that add up fast.
Fixing them reduces administrative stress and improves case flow. Here’s how to tighten your chiropractic medical billing process and keep payments coming in without unnecessary headaches.
Some claims never leave your system, creating an invisible revenue drain. They get stuck due to missing details or software misconfigurations, and you assume they’ve been sent—but they haven’t.
Fix It: Create visibility into your claim submission process with these approaches:
The best claims system in the world won't help if your claims never leave the building. Regular monitoring ensures nothing falls through the cracks, and establishing clear responsibility for tracking unsubmitted claims ensures accountability.
Also Read: Must-Have Features of Medical Billing Software for Healthcare RCM
Billing success depends on accurate coding. Get it right, and the claims process smoothly. Get it wrong, and denials pile up. Missing modifiers or incorrect codes can trigger automatic rejections, costing time and revenue. Each insurance carrier has its own rules, adding to the complexity.
For example, UnitedHealthcare rejects 97014 for electrical stimulation but accepts G0283. Using the wrong code leads to unnecessary denials and extra work.
Fix It:
You can use Noterro to add insurance codes like Modifiers and ICD to avoid any mistakes while billing.
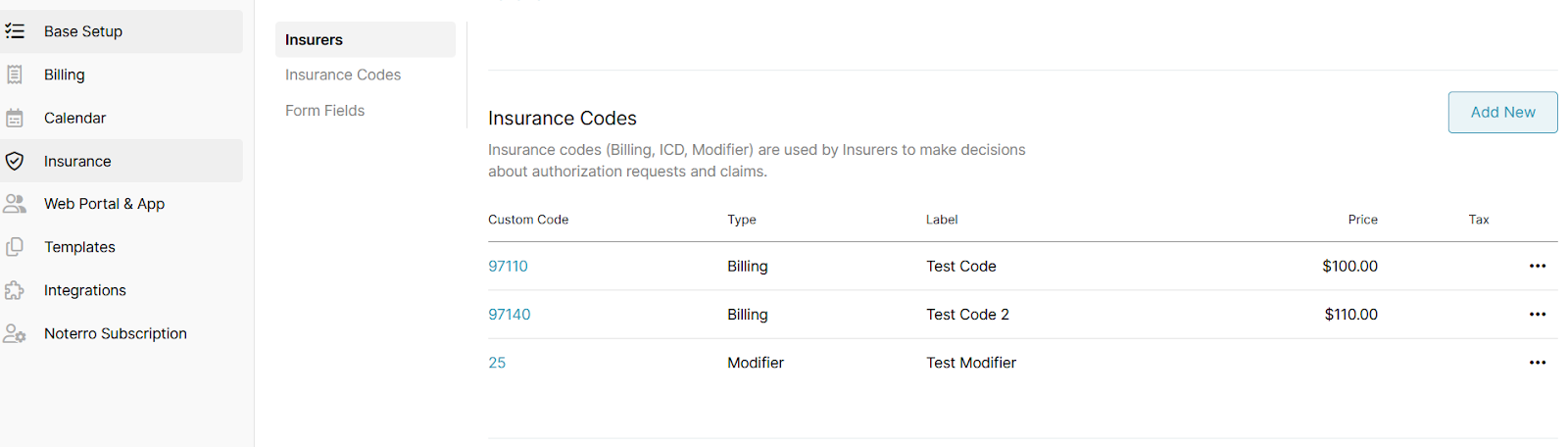
Small mistakes in coding lead to big revenue losses. You should avoid these billing and coding red flags to get payments faster.
You might also like to read: Insurance Code Recommendations for Your Invoices
Verifying coverage isn't just a good practice—it's essential for maintaining healthy cash flow. Yet many practices check insurance only at a patient's first visit, missing important changes.
Providing treatment without verifying current insurance coverage or obtaining necessary pre-authorizations leads to unpaid claims and frustrated patients.
Insurance details can change monthly, and authorizations expire without notice. Without regular verification, you're essentially providing care with no guarantee of payment.
Helpful read: Transform Healthcare Finance with Electronic Medical Billing Solutions
Timing matters in billing for chiropractic services. The longer you wait to submit claims, the longer you wait to get paid—it's that simple.
Many clinics batch claims weekly or monthly, creating unnecessary delays in payment and increasing the risk of timely filing issues.
This practice essentially provides insurance companies with an interest-free loan of your money. Meanwhile, your practice bears the burden of delayed cash flow.
Fix It:
Faster claim submissions mean faster payments. Don’t let delays in your process turn into delays in your revenue.
A small mistake—like a missing digit or incorrect modifier—can turn a valid claim into a denial nightmare. Fixing rejected claims takes more time and effort than submitting them correctly the first time. Prevention is always faster than correction.
Fix It:
When claims are denied, the clock starts ticking. Every payer has specific timeframes for appeals, and missing these windows means losing your right to payment.
Many practices delay follow-up on denied claims—or worse, never appeal them at all—resulting in significant revenue loss.
According to industry data, 60% of denied claims are never resubmitted. This represents pure revenue loss for services you've already provided.
Solution:
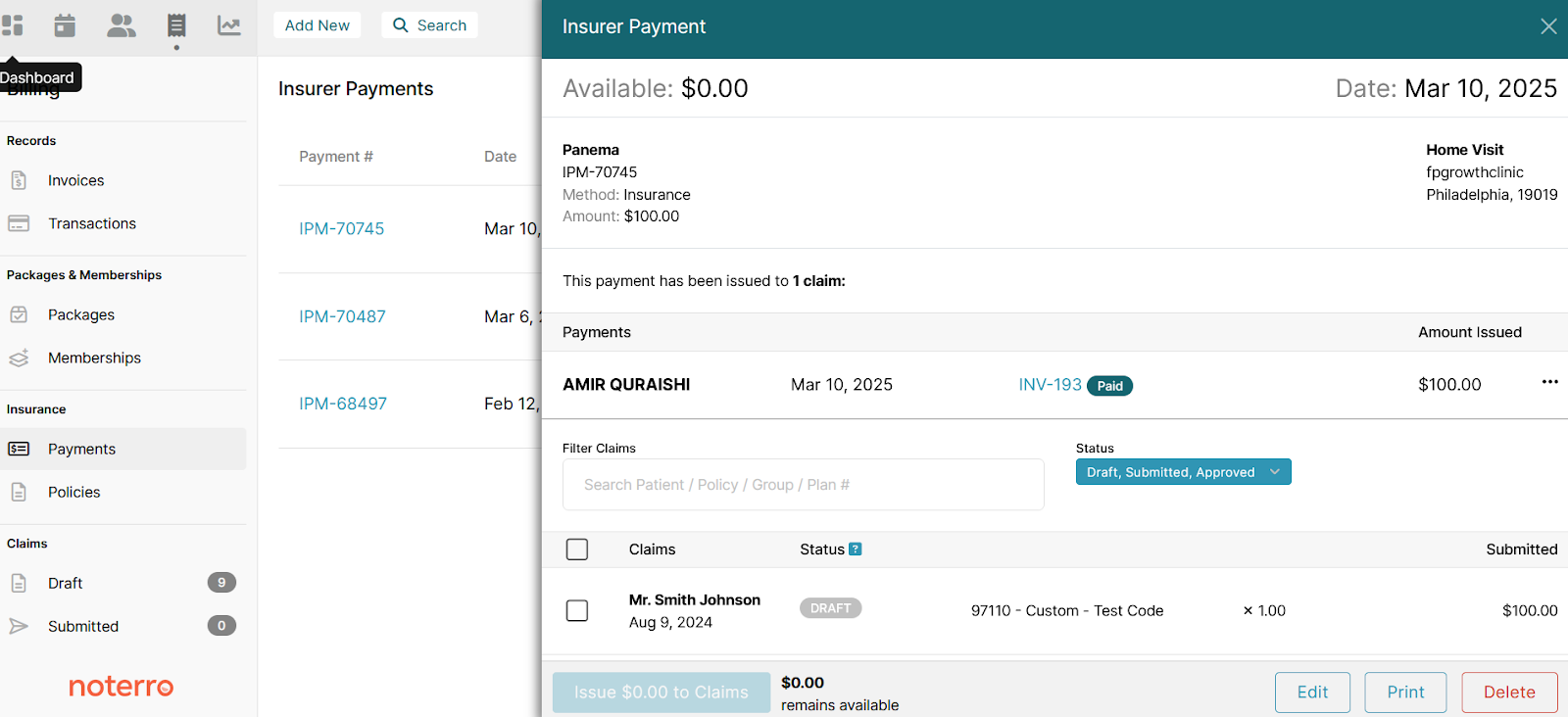
Manual payment posting isn't just time-consuming—it's prone to errors that can create accounting nightmares and incorrect patient balances. It leads to discrepancies, reporting inaccuracies, and missed collection opportunities.
When payments aren't properly reconciled with claims, your financial reports become unreliable, making it difficult to identify true collection issues.
Solution:
Interesting read: Empower Your Chiropractic Practice with Effortless Billing Solutions
Your accounts receivable represents money earned but not yet collected. The longer a claim remains unpaid, the less likely you are to ever receive payment.
Many clinics allow unpaid claims to linger for months, significantly reducing the probability of collection. Every day an unpaid claim ages, your chances of collection diminish.
Solution: You need to implement proactive A/R management in which you:
The revenue cycle begins the moment a patient schedules an appointment. Your front desk team plays a critical role in preventing billing problems before they start.
Many payment errors originate at check-in, with incorrect insurance information, missing demographics, or uncollected copays.
Solution:
Your next read: The Comprehensive Growth Plan for Chiropractic Practices: From Startup to Scalable Success
Manual processes simply can't keep pace with today's complex billing requirements. Modern software solutions automate repetitive tasks while reducing human error.
Outdated or paper-based systems slow down reimbursements and increase error rates.
Every manual step in your chiropractic medical billing process represents an opportunity for mistakes and delays. Technology can eliminate many of these vulnerabilities while speeding up your entire revenue cycle.
Solution:
Billing shouldn’t be a constant headache. With the right chiropractic billing tips, you can reduce denials, speed up payments, and free your team from unnecessary admin work.
Even small changes—like catching claim errors early or submitting claims faster—can have a big impact on cash flow and efficiency.
By applying these strategies, you can:
For a smarter, more efficient process, Noterro helps at every step. From CMS-1500 exports for US users and TELUS eClaims integration for Canadian clinics to automated follow-ups and real-time claim tracking, it ensures you stay on top of your revenue cycle with less effort.
Billing success isn’t about a complete overhaul—it’s about consistent improvements. Start with what impacts your bottom line the most, and build from there. The right systems and tools make all the difference.
For patients with high deductibles, set clear payment expectations upfront. Offer pre-treatment cost estimates, flexible payment plans, and digital payment options. Consider automating patient reminders for outstanding balances to avoid delayed collections.
Regularly review Explanation of Benefits (EOBs) to catch underpayments. Use billing software that provides variance reports comparing expected vs. actual payments. Noterro’s real-time payment tracking helps identify discrepancies so you can dispute incorrect reimbursements promptly.
Ensure each provider uses consistent documentation and coding practices by implementing standardized billing workflows. Assign a billing lead to review claims for accuracy before submission. Using a centralized system like Noterro helps manage provider-specific billing rules efficiently.
Track payment timelines for each insurer and set escalation procedures for delayed claims. If a payer consistently delays reimbursements, follow up aggressively with documented proof of submission dates. Consider joining a provider advocacy group or negotiating contracts to avoid recurring payment bottlenecks.
Tags



