End-of-Year Sale: Subscribe by December 31 to Get 3 Months Free!
Learn More
Table of Contents

Experience Better Practice Management Today!
Starting at $28.05/month
No Credit Card Required

Experience Better Practice Management Today!
Starting at $30/month
No Credit Card Required
Chiropractic billing looks simple on the surface, but it doesn’t take long before the little things start slowing you down. A missed detail during intake, a code that hasn’t been updated, or a note that needs one more line.
Then an EOB comes in, and something doesn’t add up. Before you know it, you’re fixing claims instead of focusing on patients.
The clinics that stay steady figured out a few things early on.
When these habits fall into place, billing gets lighter. Payments come in on time. Denials drop. And your team finally gets a chance to catch their breath.
In this guide, I’ll walk you through the chiropractic insurance and billing tips I share with clinics. They’re practical, simple, and effective in real-world settings where time is tight and accuracy is crucial.
Over the years, I’ve seen a few habits make the biggest impact on billing. Here are the ones I recommend to every chiropractic clinic I work with.
Most billing problems start at the front desk. If a patient’s insurance details are wrong or incomplete, everything that follows is built on a bad foundation. This is one of the biggest reasons claims get denied.
Before every visit, check the patient’s eligibility, policy number, plan type, and coverage limits. Make sure their authorization hasn’t expired. You’d be surprised how many denials come from something as small as a typo in a policy number or a missed renewal date.
If you use digital intake forms from Noterro, the process becomes much cleaner. The policy information goes directly into the patient’s profile, and the team isn’t retyping details that can introduce errors. It saves your staff time, and more importantly, it reduces the number of claims you have to correct later.
Coding mistakes cost clinics more money than most people realize. The codes you submit need to match what was done, why it was done, and what the diagnosis supports. Even a small coding error can push a claim into the denial pile.
Stay updated with current CPT and ICD-10 codes. It helps to keep a short list of the codes you use the most. For most chiropractors, that includes CPT 98940 to 98942 for adjustments and 97140 when you add manual therapy.
These codes need the right diagnosis and the right modifier when required. If the modifier doesn’t match the clinical picture or the payer’s rule, the claim gets held back.
The 2025 to 2026 updates brought changes that affect how chiropractic services are reported, especially around therapy codes and time-based billing. If you haven’t reviewed those updates yet, put them on your list. Staying current is one of the quickest ways to reduce denials.
Another thing many clinics miss is payer-specific rules. Some insurers want a certain modifier attached to a therapy code. Some want a diagnosis listed first. Some want an additional note in the claim. If your codes are correct but don’t match the payer’s preferences, the claim can still get stuck.
A simple monthly check helps. Take the codes you use all the time and make sure nothing changed. Make sure your team is using the same information as you.
Insurance companies want notes that clearly support what you billed. When your SOAP notes miss details or feel rushed, the claim becomes harder to defend. I’ve seen this slow clinics down more than anything else, and it’s usually avoidable.
Strong documentation doesn’t mean writing more; it means writing clearly. This is where Noterro can help. Its SOAP note template helps you stay consistent even on busy days. Snippets shave time off repeat phrasing, and you can use predictive charting to boost when you’re trying to stay on track between appointments.
There are days when typing is the last thing you want to do. That’s when voice-to-chart Scribe in Noterro help you finish your notes without losing accuracy.
Every clinic deals with denials, but most denials could have been prevented. The most common issues come from:
A simple pre-check process can save you hours later. Before submitting any claim, confirm the patient’s information matches the insurer’s data, the diagnosis supports the procedure, and the documentation is complete.
A small improvement in your denial rate makes a real difference. Even a one percent improvement adds up to thousands of dollars every year for most clinics. It also reduces the stress on your staff, who won’t have to redo the same work twice.
Trying to track claims manually is one of the fastest ways to fall behind. On a busy day, it’s the task that gets pushed aside. Batch submissions help you send more claims at once, and daily reviews help you stay on top of what’s still pending.
Submitting claims through Availity in Noterro keeps everything moving without the usual back-and-forth. Digital submissions go out clean, and you see updates sooner. You know right away if a claim was accepted, denied, or needs a quick fix. No guessing and no waiting for someone to check another portal.
When your billing software connects directly to insurers, the whole process becomes simpler. You can see every claim in one place, resubmit with a couple of clicks, and avoid bouncing between portals just to know what’s going on.
Insurance policies and coding rules change every year. Even small updates can create problems if your team isn’t aware of them. Build time into your schedule for short training sessions. A quick update every quarter helps your team stay consistent.
Cross-train staff members so no single person becomes the only one who understands how billing works. This is especially helpful in small clinics where one person often wears many hats.
You can also create a shared billing playbook for your clinic and keep it simple. Add your most common codes, your modifiers, your payer rules, and anything your front desk needs to check during intake. This reduces mistakes and gives new staff a place to start.
EOBs confuse a lot of people, even practitioners who have been in the field for years. If you can’t read your EOBs clearly, it becomes harder to know whether you’ve been paid correctly.
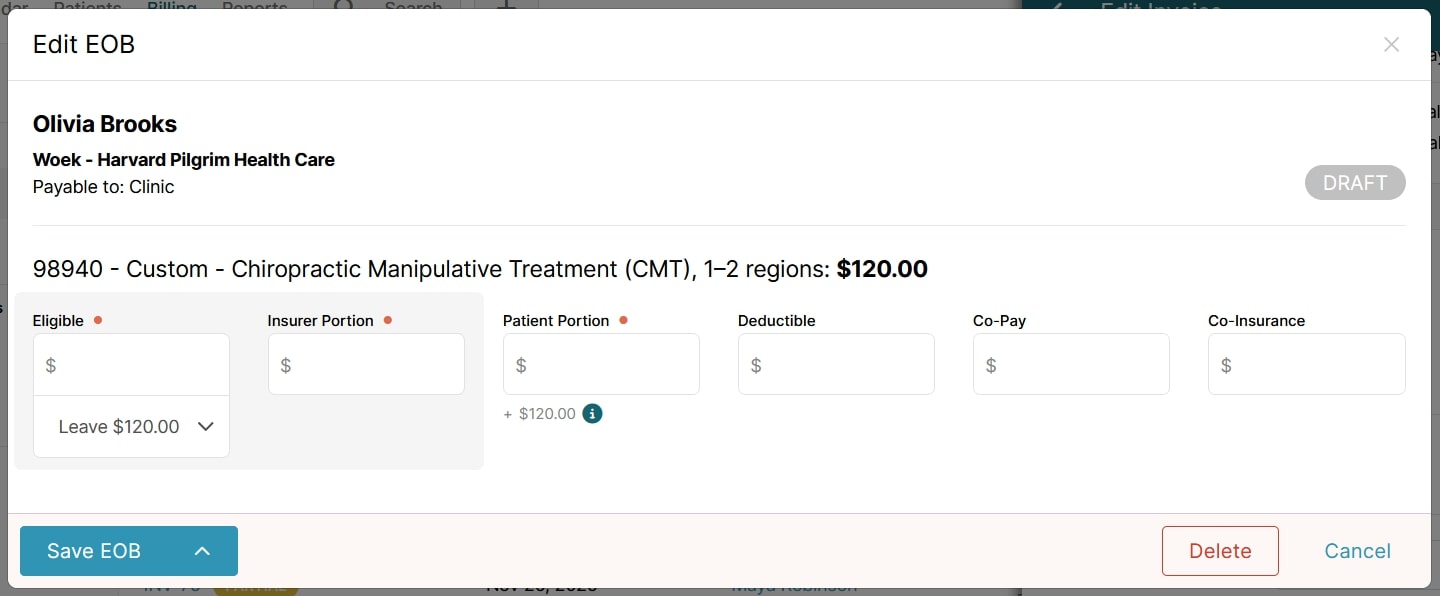
A chiropractic EOB shows how the insurer processed the claim. Understanding the parts of an EOB helps you catch underpayments or errors before they snowball.
EOBs in Noterro make it easier to break down what happened with a claim. You see the procedure, the billed amount, and every portion that needs to be assigned. You can add the eligible amount, the insurer’s portion, the patient’s portion, and any deductible, co-pay, or co-insurance that applies. It lays everything out in one place so you can record the payment exactly as it came through.
When you update an EOB, the service details and the payable information stay visible, and you can save it as a draft until everything is confirmed. This helps you avoid mistakes and gives you a clear record you can refer to later.
Having all of this in one screen reduces guesswork and keeps you from bouncing between spreadsheets or separate tools. It makes it easier to stay accurate, close out claims faster, and keep your billing organized.
It’s hard to improve your billing if you aren’t watching the right numbers. A few metrics can tell you exactly where things are slowing down.
Keep an eye on your days in accounts receivable, your first pass claim rate, your denial percentage, and how long each payer takes to reimburse you. These numbers reveal issues long before they turn into bigger problems.
Noterro makes this easier because your reports all live in one place.
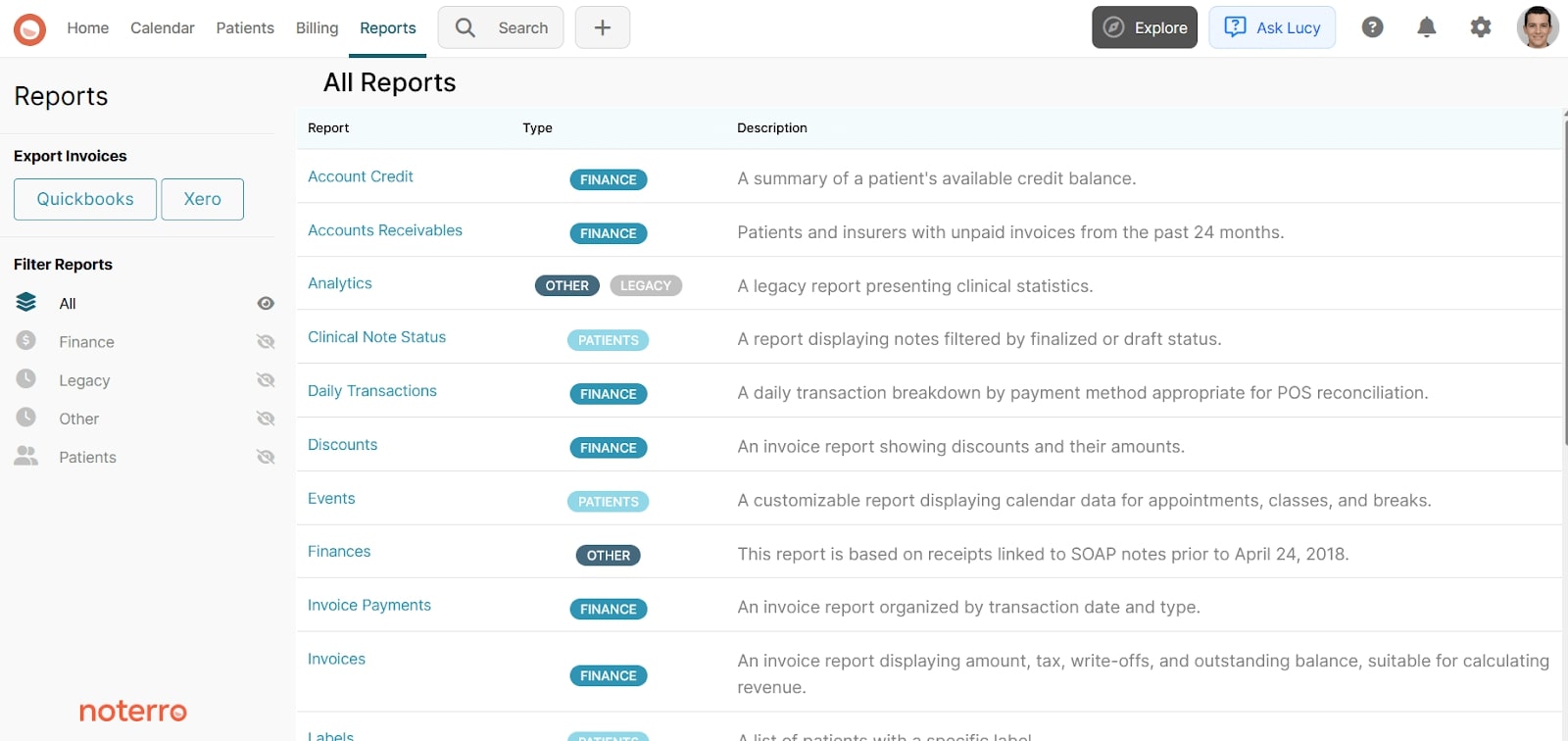
When these reports are easy to access, you spend less time digging for information and more time fixing what needs attention. It’s a simple way to keep your billing healthy and your revenue steady.
Chiropractic billing gets a lot easier when the basics are solid. Verify the right details at the start, use the right codes, and keep an eye on the numbers that show how your billing is really doing.
If billing feels heavier than the care you give, something’s off. You don’t have to rebuild everything at once. Pick one part of your workflow, clean it up, and move to the next. Small changes add up fast.
And if you want a simpler way to manage all of this, Noterro can help. Your claims, payments, notes, and patient records all live in one place so your team isn’t chasing information all day. You can try it free for 14 days without a credit card.
Your time should go toward helping patients, not paperwork. Let’s make sure your billing supports that.
Tags



