End-of-Year Sale: Subscribe by December 31 to Get 3 Months Free!
Learn MoreTable of Contents

Experience Better Practice Management Today!
Starting at $28.05/month
No Credit Card Required

Experience Better Practice Management Today!
Starting at $30/month
No Credit Card Required
If you’ve ever finished a session knowing you did good work, only to have the claim denied later, you’re not alone. It’s frustrating. Most of the time, the issue isn’t with you but how it was billed.
Insurance companies don’t read SOAP notes like we do. They’re scanning for CPT codes. These are five-digit codes that explain what kind of treatment you gave.
There’s a specific code for every massage, from Swedish massage and targeted soft tissue work to rehab exercises. And if your notes don’t match the code or the code isn’t documented correctly, you don’t get paid.
Let’s break down the most-used CPT codes for massage therapy insurance billing. I’ll also walk you through when to use them, what kind of documentation matters, and how to avoid common mistakes that lead to denials.
There are a few core codes that come up again and again in massage billing. Let’s unpack what they mean, when they make sense to use, and how to make sure your notes fully support your claims.
This is probably the most common Massage CPT Code you’ll use. It covers Swedish massage techniques; think effleurage (gliding), petrissage (kneading), and tapotement (rhythmic tapping).
It’s the go-to when your session focuses on improving blood flow, easing general muscle soreness, or reducing stress and tension.
For instance, let’s say someone books in after a week of poor sleep and long hours at the desk. You run a 30-minute Swedish massage session on their back and shoulders to improve circulation and help them relax. That’s 97124.
This code is billed in 15-minute units. So if you work for 45 minutes using only Swedish massage, that’s three units.
But you need to write down what areas you treated, the techniques you used, and what outcome you were targeting. Even if your work helped, unclear notes will hold up payment.
This code is for more focused, problem-solving work. You’re not just relaxing tissue but addressing specific issues like joint stiffness, fascial restrictions, or chronic pain points.
For example, if a client comes in with a frozen shoulder, and you spend 15 minutes applying sustained pressure to the subscapularis or use a pin-and-stretch technique on the pec minor to improve joint mobility, that’s 97140.
Same goes for trigger point therapy or any soft tissue work that’s part of a treatment plan. Like 97124, this is also a 15-minute timed code.
But you can’t bill it for the same area at the same time as 97124. So if you’re doing Swedish massage on the upper back and manual therapy on the left shoulder, be specific about it in your notes.
Use this one when you’re helping a client re-learn or improve movement patterns. It includes balance training, posture correction, or activities that improve coordination between the brain and muscles.
For instance, let’s say you’re working with a client who’s recovering from a foot injury and has poor ankle stability. You guide them through balance work on a wobble board and reactive drills for proprioception. That’s a great fit for 97112.
It’s also a timed code in 15-minute units. In your documentation, explain what activities you used, what movement goal you were targeting, and how the client performed.
This one’s a bit more straightforward. If you apply moist heat or cold packs as part of your treatment, this is the CPT code for it.
Let’s say you apply a hot pack before treatment to relax muscles, or use cold afterward to reduce inflammation. Just know it’s an untimed code, so, you bill it once per session, regardless of whether you apply it for 5 minutes or 20.
Many insurers see it as bundled with manual therapy codes, so don’t always expect reimbursement unless the client’s plan specifically allows it. Still, it’s good practice to document its use.
This is massage therapists’ go-to when they are working with clients on active, therapist-led exercises. That includes stretching routines, resistance work, or exercises to restore range of motion.
For example, a client is rehabbing from shoulder surgery and you guide them through resisted external rotations, band pulls, and mobility drills for scapular stability. Again, this is a 15-minute timed code. Your notes should detail what exercises you did, how they were performed, and what specific outcome you were aiming for.
Now that we’ve covered the common codes, let’s look at how timing plays into billing
Also read: Top 8 Medical Billing Software to Simplify Your Practice in 2025
Let’s talk about timing. Most CPT Codes for Insurance Billing follow the 8-minute rule. That means you need to provide at least 8 minutes of service to bill 1 unit.
Here’s the breakdown:
If you only spend 7 minutes on a treatment, you can’t bill for it. That’s why tracking start and stop times is a habit worth forming. Write it down while it’s fresh—it’ll save you from second-guessing later.
Next, let’s go over modifiers, those little add-ons that can make a big difference.
Modifiers are easy to overlook, but they help explain what happened in a session. Here are two you’ll want to keep on hand:
Modifiers tell the insurance reviewer what actually happened. And in a system that often works off checkboxes, these small details can help your claim go through the first time.
Let’s zoom out a little. Before you even bill, it’s good to know what’s actually covered.
This part can get tricky. Not every insurance plan covers massage therapy, and when it does, there are often hoops to jump through.
Most plans require proof of medical necessity. That means pairing the right CPT Code for massage therapy with an appropriate diagnosis code. In some cases, you’ll need a physician referral or pre-authorization.
Here’s what I recommend checking before billing:
Now let’s talk about documentation. It’s what ties everything together.
Also read: Streamline Client Care with Massage Therapy SOAP Notes Software
Every code you use should be backed by your notes. If it’s not documented, it didn’t happen. And when insurance reviewers check, they want detail, not generalizations.
Your notes should include:
Instead of saying “client felt better,” try “client reported decreased pain in lumbar spine from 6/10 to 3/10 after trigger point release.” That level of specificity helps you get paid and protects you if you’re ever audited.
This is where Noterro, a holistic practice management software, can really help. The SOAP notes feature is structured to guide you through what insurers want to see. You can document by area, technique, and outcome, all while staying organized in the client record.
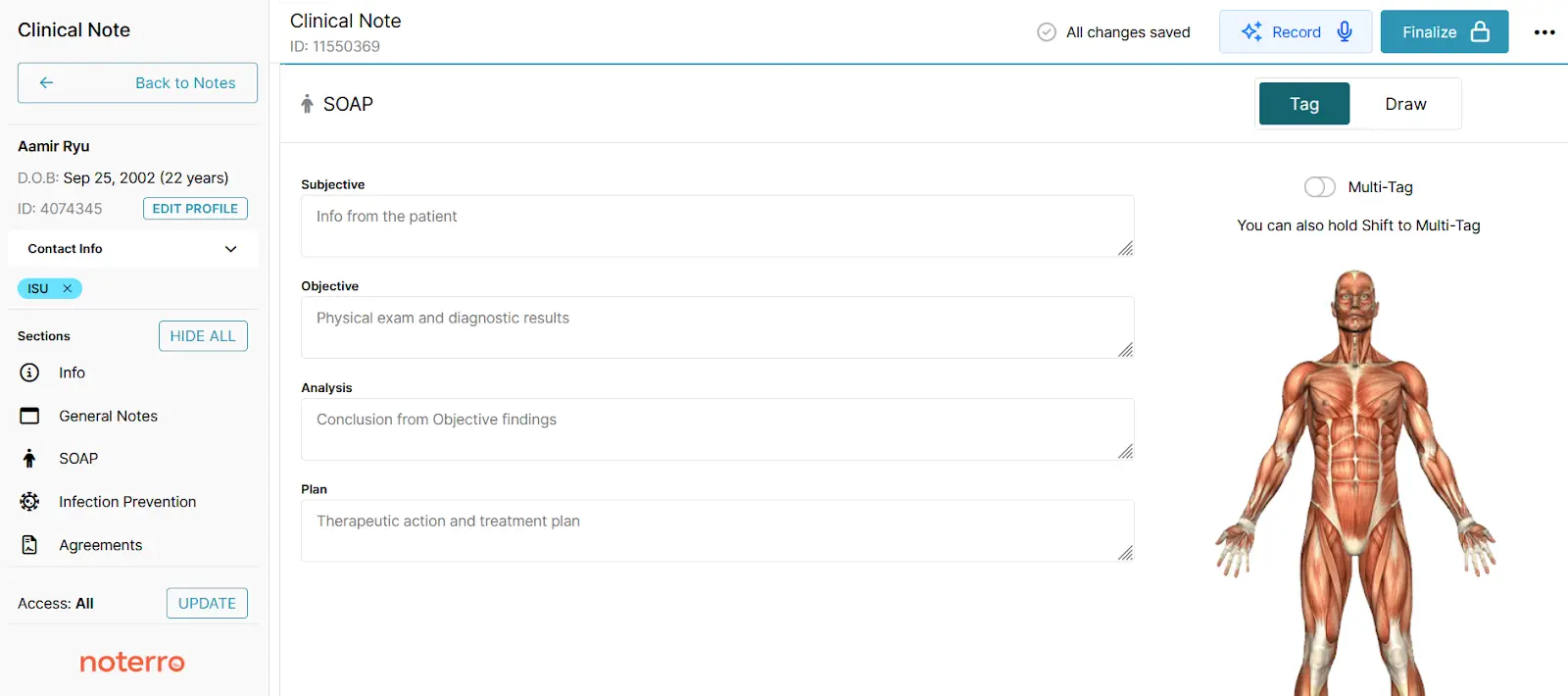
If you’re someone who prefers speaking over typing, AI Scribe lets you record your session notes on the fly. It transcribes your voice into clean, professional notes you can use for claims. That means less time at the keyboard, fewer errors, and better reimbursement odds.
You’ve got the codes and documentation. Now let’s make sure your claims don’t get stuck in limbo.
Bonus read: 7 Essential Tips to Speed Up SOAP Note Writing Efficiently
Denials are common, but often avoidable. I see a few issues come up repeatedly:
My advice? Take five minutes before submitting a claim to double-check everything. You’ll save yourself a lot of time chasing denials later.
Insurance billing is not simple, but it doesn't need to dominate your day either. Using the correct CPT codes, documenting nicely, and pre-billing preparing just a bit can keep you out of the back-and-forth with insurers.
And if the admin work still doesn't feel light? That's where Noterro’s massage therapy software comes in. It's designed with features that actually match how you work, such as organized SOAP notes, integrated timers, and AI Scribe for speedy voice-to-note recording.
It's there to assist you to get paid quicker and spend more time with clients, not running after paperwork.
Tags



