End-of-Year Sale: Subscribe by December 31 to Get 3 Months Free!
Learn More
Table of Contents

Experience Better Practice Management Today!
Starting at $28.05/month
No Credit Card Required

Experience Better Practice Management Today!
Starting at $30/month
No Credit Card Required
Starting your practice is exciting. But billing and insurance?
That’s where many new practitioners get stuck.
If you don’t set up clear systems early, you’ll spend more time chasing payments than treating patients. I’ve often seen that billing feels overwhelming until you have the proper setup.
Here are a few things that make the most significant difference when you’re starting:
Of course, knowing what to do is one thing, and figuring out where to start is another. So, let’s take it from the top.
Most practitioners say the clinical side feels natural, but the admin side quickly becomes overwhelming. Billing, insurance claims, and payments are the areas that cause the most stress.
Here are some of the common roadblocks:
These challenges are common but can be solved with the right systems and integrations.
In the following sections, I’ll walk you through how to handle each one, from managing insurance claims to deposits, card payments, and billing best practices.
Insurance billing is often the most challenging part of running a new practice. Getting it wrong delays payments and adds unnecessary stress. Here’s how to keep it manageable:
Every claim should be tracked from submission to payment. Missing a step often means money left on the table. With Noterro’s TELUS eClaims integration, Canadian clinics can process claims directly in the system, cutting down on manual entry and reducing errors.
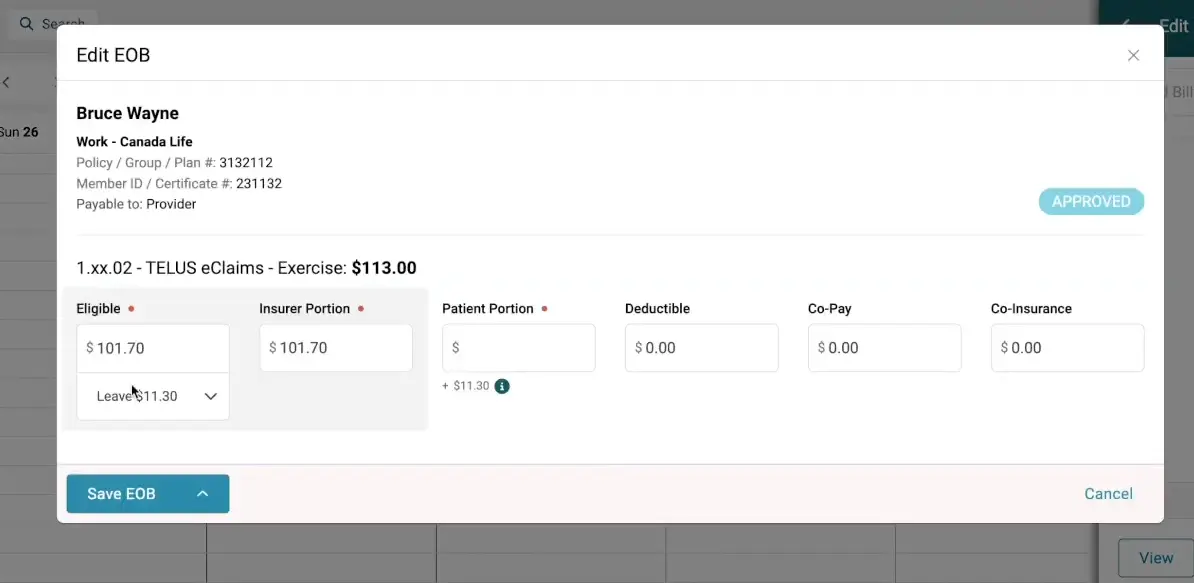
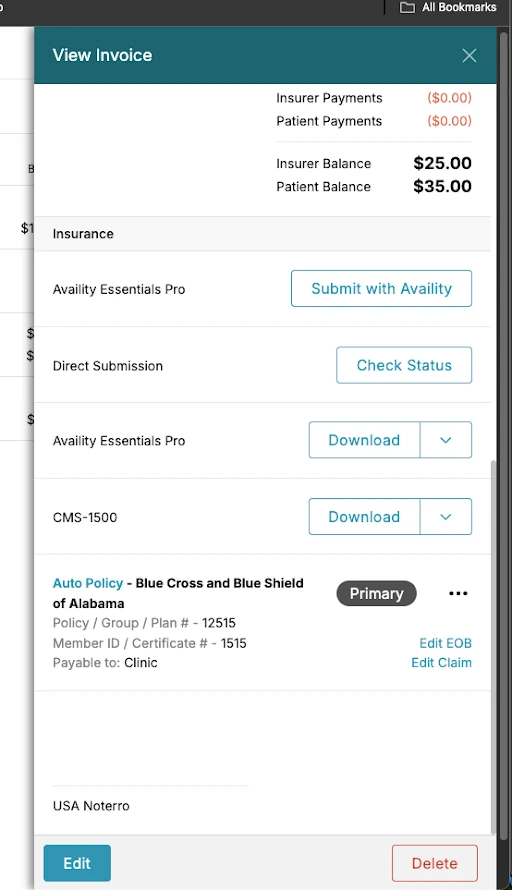
For U.S. clinics, Noterro integrates with clearinghouses like Availity, Office Ally, or TriZetto, making it easy to prepare claims in batches. For example, you can group your draft claims, say, at the end of the week, export them as a single EDI file, and upload them in one step. This workflow keeps submissions fast, organized, and consistent.
Before you provide care, confirm that a patient’s insurance plan covers your services. This prevents denied claims and avoids billing surprises for patients. With Noterro’s integration with Availity in the U.S., eligibility checks are quick and accurate, though claims still need to be submitted separately. Once claims are sent, don’t assume payment is automatic; regularly check their status and follow up on outstanding ones.
Noterro gives you visibility into the status of your claims, so nothing slips through. In Canada, TELUS eClaims allows the same process from within Noterro, letting you submit and track claims directly without leaving the system.
Noterro is directly integrated with Availity Pro, allowing you to submit claims seamlessly from within the platform. Alternatively, you can generate an EDI file from an individual invoice or as part of a batch and then log in to your clearinghouse portal to upload the file for processing.
One U.S. chiropractor who processes more than 200 claims per week used to manage everything in spreadsheets. Claims were often lost, payments were delayed, and reconciling accounts took hours.
After switching to Noterro, they could track each claim from submission to payment, clearly see statuses like submitted, approved, or rejected, and run receivables reports by patient and insurer. What used to be chaotic is a predictable process that saves weekly hours.
While insurance claims are often the biggest billing challenge, they’re not the only one. Even with claims handled, you still need a reliable way to manage direct payments.
In this blog, I also discussed the credentialing process for chiropractors with insurance companies in detail. Check it out!
Patients expect flexibility, whether they’re paying per visit, on a recurring schedule, or as part of a membership. At the same time, your clinic needs clear agreements in place to avoid confusion and protect cash flow. That’s where stored cards, memberships, and signed policies come in.
With Noterro’s Square integration, you can map a card to a patient profile and charge it for future invoices. Noterro does not store credit card details. All cards are stored securely with the payment processor. When you add a card to a profile, it’s linked to the processor’s stored record.
The fastest way to use this is through the “Store or Map Card” option on a patient profile when processing an invoice. It saves time at checkout and keeps payments simple for patients.
Pro Tip:
Stored card transactions often come with slightly higher processing fees. To keep billing smooth, build those costs into your service pricing so patients don’t see a separate fee.
Recurring payments in Noterro are part of membership billing. You can set up memberships so payments run automatically on a schedule. Using Square, these payments are processed securely, keeping memberships active without manual billing. This reduces missed payments and cuts down on admin work.
Also read: How Memberships Drive Patient Retention in Chiropractic Clinics
You can add agreements and consent forms directly to a patient’s profile in Noterro. Specialized widgets on your forms create policies automatically when a patient completes them.
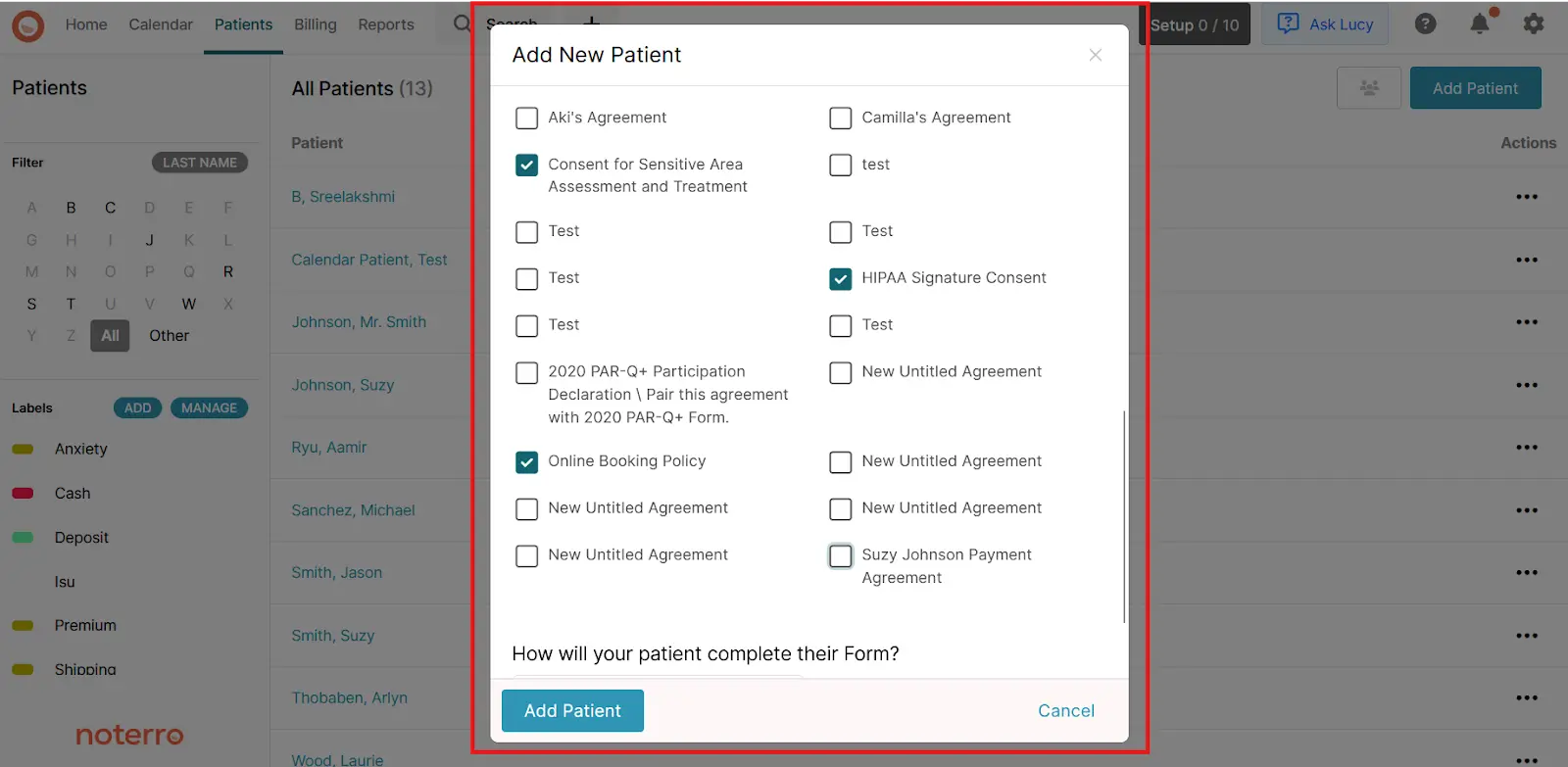
Consent agreements, payment authorizations, or direct billing authorizations can be collected upfront. Once submitted, they’re attached to the profile, so everything is stored in one place and easily referenced.
With cards, memberships, and agreements in place, your payments stay consistent, and billing becomes easier to manage. However, payments are only one part of the picture. You need insurance and clinic billing to work together to make billing truly efficient.
Many new clinics try to keep insurance and billing separate. It almost always creates extra work and leads to mistakes. Linking the two makes the process faster and more accurate.
With Noterro, practitioners can manage claims through Availity, Office Ally, and Trizetto without re-entering data. In Canada, TELUS eClaims adds real-time claim tracking. In the U.S., follow-ups still need to be done through the clearinghouse, but submissions are quick and organized. That means reimbursements come in faster and cash flow stays steadier.
When insurance and billing work together, clinics spend less time buried in admin and more time focusing on patients.
If you’re a massage therapist, you can check this blog on how to keep billing & insurance stress-free.
The next step is protecting your time and cash flow on the front end, starting with how you handle deposits.
Deposits give your practice added security. They reduce no-shows, protect your time, and help secure future appointments. For new practitioners, deposits can also keep cash flow steady in the early months of running a clinic.
How can Noterro help here?
With Noterro, you can require patients to pay a deposit when booking online. You can even set deposit amounts by service, so a portion of the fee is collected upfront before the appointment.
This improves your cash flow and helps patients commit to the care they scheduled.
Here’s an example. A massage therapist I spoke with struggled with last-minute cancellations that left their schedule empty. After setting up deposits through Noterro, their cancellation rate dropped dramatically.
Patients respected the therapist’s time, and days weren’t wasted on empty slots. That simple change steadied income and made the schedule more predictable.
Here are a few best practices I’ve seen work well:
Cards, memberships, and agreements keep payments consistent, but systems only work if you build the proper habits around them.
Chiropractors can also check out my other blog on the billing issues and their fixes for their chiro practice.
Getting billing right early sets the tone for how your clinic runs. Over the years, I’ve seen new practitioners avoid a lot of stress by building these habits from the start:
Building good billing habits early will save you time, reduce stress, and keep your practice financially healthy.
Starting a clinic comes with plenty of moving parts, but billing, insurance, and payments are the pieces that hold it all together. Get them right early, and you’ll save yourself from late reimbursements, awkward payment conversations, and hours of extra admin.
What I’ve seen work best is simple: set up systems that keep your billing organized, clear your payment terms, and ensure your insurance claims don’t slip through the cracks.
That’s precisely the thinking behind Noterro. We built it so practitioners could spend less time billing headaches and more time treating patients. If you’re ready to put the proper structure in place from day one, Noterro can help you.
The best way to stay compliant is to keep accurate records and follow insurer guidelines closely. Use the correct CPT codes, document all services, and make sure claims include every required detail before submission. Regulations change, so review insurer updates regularly and adjust your process. Having written policies for billing in your clinic also helps keep staff consistent.
Start with clear agreements before care begins. When disputes come up, stay professional and empathetic. Walk patients through the charges, explain your policies, and point to the signed agreements. Document the conversation and always follow up. Patients appreciate transparency, and it prevents minor issues from turning into bigger conflicts.
First, review the rejection notice carefully to understand why the claim was denied. Common issues include missing details, incorrect codes, or eligibility mismatches. Correct the error and resubmit as soon as possible. If the claim should have been covered and no error exists, contact the insurer directly for clarification. Keeping organized records makes this process much faster, since you can quickly provide the information insurers request.
Tags



